The following studies serve as a bit of a proof of concept for adult bone length increase by showing that the two most distal of the three finger bones can increase in length with age and that the skull bone can increase in length.
Here are some selections from a statement by Roy Wuthier, a retired scientist in regards to non-growth plate methods of bone growth:
"Not all bone growth occurs via growth plate-dependent mechanisms. The growth of phalanx bone apparently is not totally dependent on growth plate elongation. As you realize, appositional growth can be mediated via osteoblasts that reside under the periosteal membrane. Thus in phalanx bones, both types of bone growth must contribute to their expansion during overall skeletal growth."<-so perhaps on the proximal end of the phalanx bone there may be a periosteal membrane despite being separated by articular cartilage.
"During typical long bone growth (elongation), you will note that the ends of the long bones (where the growth plates reside) have a larger cross-sectional area than occurs at the mid-shaft. The cells that sculpt the shape of the long bones are the osteoclasts which have the ability to remove bone. In fact in a genetic disease where osteoclast formation is suppressed, the shape of the long bones is almost "post-like" with no reduction in mid-shaft cross-sectional area."<-Perhaps the larger cross-sectional area of the epiphysis formed by growth plate growth facilitates osteoclast absorption. Thus, osteoclasts may be able to remove bone that is generated by endochondral ossification at a fast enough rate such that there is no net bone length increase. And, in ends of the bones not formed by growth plates don't have as large a cross-sectional area favoring absorption thus apposition at the ends of the bones is greater than osteoclast resorption.
A way to test this is with osteoclast inhibitors however articular cartilage endochondral ossification is slow and osteoclasts are needed for many functions. You could elevate HGH levels which increases both bone formation and resorption thus allowing you to safely lower osteoclast levels. HGH would also increase the rate of the growth so it could occur in a reasonable time frame. And then see if articular cartilage endochondral ossification could make you taller.
Metacarpophalangeal length changes in humans during adulthood: A longitudinal study
Metacarpophalangeal refers to hand bones essentially.
"Total lengths of the 19 diaphyseal hand bones were measured from standardized radiographs of healthy American whites as young adults (ca. 21 years) and again at ca. 55 years of age. The four hand-bone rows exhibit distinctive length changes: Distal and middle phalanges continue to increase significantly in length{the distal phalange may have periosteum at the distal end of the bone so it may be able to grow by appositional growth but that is not true of of the middle phalange}, proximal phalanges constitute a transition zone of little change, and metacarpals uniformly decrease in length[there are three bones in a non thumb finger. The end bone is the distal bone and the one closest to the the end is the proximal phalange. The metacarpals are part of the hand.]. Clear-cut sex differences are noteworthy: Males change more (lose more in some bone rows, gain more in others) than females. Progressive elongation was greatest in the distal phalanges where apposition around the distal aspect (“tufting”) is not constrained by a joint or epiphysis. Loss of bone length in the metacarpals by subchondral resorption is consistent with documented reductions in activity levels and grip strength with age, as well as diminished joint spaces which alter loading of the joints."
The increase in bone length was about 0.34 mm per decade.
"To test for [the possibility that the bone length gain was due to residual gain due to growth plate growth], we partitioned the sample into those cases whose younger-adult age at examination was less than 25 years and those with a radiograph after 25 years of age. Using a two-way factorial analysis of variance, grouping by age grade and sex, none of the 19 tests achieved statistical significance. "
"In the distal and middle phalanges most of the increase was accounted for by progressive apposition at the distal, epiphysis-free ends of the bones"
If you look at the phalanx x-rays you can see that distal ends of the bones do not have a growth plate.
Only the proximal(closest to the body) side has growth plates. Maybe bone growth can be renewed if you remove the epiphysis somehow. LSJL via fluid based shear strain may degrade some of the epiphysis allowing for new height growth.
"the distal phalanges, which exhibit appreciable increase, are unique in not being constrained distally by a joint or epiphysis"
"When cartilage thickness exceeds the critical dimensions that limit nutrition by diffusion, the cartilage cells hypertrophy and degenerate, the spaces become vascularized, and osteoblasts develop to initiate endochondral bone formation in the midst of the articular cartilage."
Age Changes in the External Dimensions of Adult Bone
"persistent physical activity stimulates bone growth in length. Among subjects who had, for occupational reasons, vigorously exercised the dominant limb (i.e., tennis players) that limb was found to be longer than the nondominant limb. Assuming that the Kleinburg people were, indeed, right handed, one can conclude that response to activity has stimulated a differential increase in length and breadth on the dominant side."
"This could include a process, such as a left-right difference in blood oxygen level, which would potentially lead to unequal bone growth"
The aging craniofacial complex: a longitudinal cephalometric study from late adolescence to late adulthood
"This was a recall study with 39 subjects (19 male, 20 female). Their lateral cephalograms taken during late adolescence (T1; mean age, about 17 years), midadulthood (T2; mean age, about 47 years), and late adulthood (T3; mean age, about 57 years) were evaluated. To test for significant differences between times, sexes, and the sex and time interaction, repeated measures analysis of variance was used. For the comparisons of time (T1 vs T2, T2 vs T3), the nominal alpha level was set at 0.01.
Skeletal changes were significant only from late adolescence to midadulthood; soft-tissue changes were significant from late adolescence to midadulthood, and mid- to late adulthood. Changes in skeletal tissues consisted of increases in sella-nasion length, midfacial length, and lower anterior facial height. Sex differences were apparent in the mandible. The women had downward and backward mandibular rotation; the men, on the other hand, had more forward rotation of the mandible and increased chin prominence. Mandibular growth was greater in the men. Changes in the soft tissues were the most remarkable and included significant thinning and elongation of the upper lip. Significant changes in the nose took place, including drooping of the nasal tip and columella, the latter leading to more acute nasolabial angles."
"The early examinations took place when the subjects were between 17 and 19 years of age. The later examinations occurred from 65 to 83 years, with an age range of 25 to 83 years at the final records"
"Humeri from a large, ossuary-derived sample are used to demonstrate that considerable size variability is introduced to transverse skeletal measurements when young adults and older adults are pooled. Humeri from young adults (epiphyseal lines still visible, N = 25) are smaller in transverse
dimensions than those of older adults (N = 300). Among left humeri, only shaft diameters demonstrate statistically significant differences. The right humeri, however, show statistically significant differences for six of the eight measurements. The increased size of the older adult humeri reflects the fact that appositional growth continues throughout adulthood. The more pronounced differences seen on the right side probably reflect developing dominance asymmetry.
Recognition of this source of intrasample variability will influence the choice of skeletal measurements used for population comparisons and/or indicators of robusticity."
"Differences in right lengths are not statistically significant, but they are great enough to arouse
curiosity. Left side lengths show virtual identity. Indeed, total length among young adults is 0.5 mm greater than that among older adults."
"subperiosteal surface apposition continues lifelong or at least through the tenth decade"
"The increases in total length and physiological length may also be tied to the continuing appositional process. Appositional increase at the articular surfaces has been cited as a possible explanation for the slight increase in total body height seen up to ages 25-30."<-I think the increase in this study is too large to be due to appositional growth.
The increase in right humeral length is huge. Much more than can be accounted for by appositional growth. Since left did not increase it furthers the likelihood of a mechanical loading driven mechanism.
This study echoes that bilateral asymmetry is contributed to by mechanical loading:
Bilateral asymmetry of the humerus during growth and development
"A large skeletal sample of nonadults from English archaeological sites was examined using standard metric techniques to assess when right-sided asymmetry first appears in the human skeleton. Results of this work indicate a change in directional asymmetry during growth and development, with infants and young children exhibiting no significant asymmetry and older children and adolescents demonstrating right-sidedness. This trend is consistent with what has been observed in previous studies of upper limb asymmetry in skeletal material and behaviorally in living children, adding further strength to the premise that biomechanical forces strongly influence bilateral asymmetry in the upper limb bones. Variability in the magnitude of asymmetry between different features of the humerus was also noted. This characteristic can be explained by differing degrees of genetic canalization, with length and articular dimensions being more strongly canalized than diaphyseal properties."
The aging craniofacial complex: a longitudinal cephalometric study from late adolescence to late adulthood
Skeletal changes were significant only from late adolescence to midadulthood; soft-tissue changes were significant from late adolescence to midadulthood, and mid- to late adulthood. Changes in skeletal tissues consisted of increases in sella-nasion length, midfacial length, and lower anterior facial height. Sex differences were apparent in the mandible. The women had downward and backward mandibular rotation; the men, on the other hand, had more forward rotation of the mandible and increased chin prominence. Mandibular growth was greater in the men. Changes in the soft tissues were the most remarkable and included significant thinning and elongation of the upper lip. Significant changes in the nose took place, including drooping of the nasal tip and columella, the latter leading to more acute nasolabial angles."
"The early examinations took place when the subjects were between 17 and 19 years of age. The later examinations occurred from 65 to 83 years, with an age range of 25 to 83 years at the final records"
"this investigation provided further evidence for the continuation of changes in the craniofacial complex with age, and it did not corroborate the
hypothesis that growth stops soon after puberty"
"Statistically significant changes occurred from late
adolescence to midadulthood and from mid- to late
adulthood. Changes in the skeletal tissues consisted of
increases in sella-nasion length, midfacial length, and
lower anterior facial height"
"From late adolescence
through late adulthood, skeletal changes included on
average a 2-mm increase in maxillary length, about a
3-mm increase in mandibular length, and about a
3.5-mm increase in lower anterior facial height."
"increase in anterior cranial
base length in their adult growth study"
"Small
increases were noted in the men from mid- to late
adulthood, and these changes were not statistically
significant. Similar findings of increases in mandibular length after adolescence were noted in previous
studies."
The papers being Facial and dental changes in
adulthood., Changes in the craniofacial complex
from adolescence to adulthood: a cephalometric study, and . Recent knowledge concerning craniofacial aging
You can see that T2 and T3 is well past skeletal maturity
Dynamic loading stimulates mandibular condyle remodeling
"We and others have reported that low-magnitude high-frequency dynamic loading has an osteogenic effect on alveolar bone. Since chondrocytes and osteoblasts originate from the same progenitor cells, we reasoned that dynamic loading may stimulate a similar response in chondrocytes. A stimulating effect could be beneficial for patients with damaged condylar cartilage or mandibular deficiency.
Studies were conducted on growing Sprague-Dawley rats divided into three groups: control, static load, and dynamic load. The dynamic load group received a dynamic load on the lower right molars 5 minutes per day with a 0.3 g acceleration and peak strain of 30 με registered by accelerometer and strain gauge. The static load group received an equivalent magnitude of static force (30 με). The control group did not receive any treatment. Samples were collected at days 0, 28, and 56 for reverse transcriptase polymerase chain reaction analysis, microcomputed tomography, and histology and fluorescent microscopy analysis.
Our experiments showed that dynamic loading had a striking effect on condylar cartilage, increasing the proliferation and differentiation of mesenchymal cells into chondrocytes, and promoting chondrocyte maturation. This effect was accompanied by increased endochondral bone formation resulting in lengthening of the condylar process.
Low-magnitude, high-frequency dynamic loading can have a positive effect on condylar cartilage and endochondral bone formation in vivo. This effect has the potential to be used as a treatment for regenerating condylar cartilage and to enhance the effect of orthopedic appliances on mandibular growth."
Continuing bone growth throughout life: A general phenomenon
"Cross-sectional data on 2799 subjects from five different populations and longitudinal data on 113 older adults indicate continuing adult bone growth in the second metacarpal. Similar 6-decade increases in the size of the cranium confirm continuing bone growth as a general phenomenon not necesarily related to weightbearing or flexion stress and representing an increase of approximately 10% in skeletal volume concomitant with the major age-associated decrease in skeletal mass."
"there is a small but completely systematic three-decade gain in metacarpal width at mid-shaft in both sexes and all five populations sampled"
The scientists reported an increase in skull length.
"Modeling-based bone formation contributes to the periosteal expansion, just as remodeling-based resorption is responsible for the medullary expansion seen at the long bones with aging."<-Can we translate this into height?
Extreme elongation of the transverse processes of the fifth lumbar vertebra: an unusual variant.
"the iliolumbar ligament does not exist at birth, but develops gradually in the first decade and attains full differentiation only in the second decade."
Mechanical strain leads to condylar growth in adult rats.
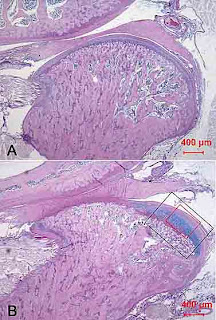
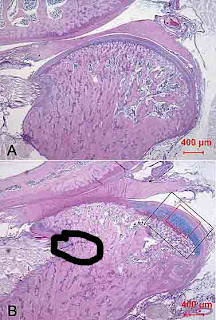
I'm planning on looking for ectopic signs of cartilage formation later as that is what we're trying to induce with LSJL. However there is some blue staining(which means it's positive for cartilage) on A but it is very faint. Note though that the entire shape of B(experimental) is different than A(control) so there must be some mechanism to achieve that.
"Alcian blue-PAS staining showing the overview of rat's TMJ condyle at age of 141-day (experimental day 21). The thickness of cartilage in the posterior condyle is remarkably increased by mandibular advancement (B) than that of control (A). Two measurement frames are illustrated on (B), one for the measurement of thickness of layers (1104×811µm, black) and the other frame for the cell counting (547×402µm, red)."
Here's the ectopic chondrogenesis highlighted with GIMP(blue line):
Here's the Col2a1 expression areas:
Here's another paper with the same author:
"The aim of this study was to determine the mandibular morphology before, during, and after bite-jumping in nongrowing species. Fifty-two adult female Sprague-Dawley rats were divided into four experimental groups and four control groups. The experimental groups were fitted with fixed bite-jumping devices that protruded the mandible. The animals were sacrificed on days 3, 14, 30, and 60. Right halves of the mandible were harvested and freed of soft tissue. Digital pictures were obtained in a standardized manner. Selected linear and angular measurements were made. There were no morphological differences between the controls and experimental group on days 3 and 14. The length of condylar process increased significantly on day 30 and remained so on day 60 in the experimental group. The angulation of the condylar process was significantly affected because of increased apposition of bone in the middle and especially the posterior parts of the condyle. Thus, bite-jumping of the mandible in adult rats affects the size and angulation of the condylar process because of differential apposition of bone on the condylar head."
Above is the condylar process.
Studies were conducted on growing Sprague-Dawley rats divided into three groups: control, static load, and dynamic load. The dynamic load group received a dynamic load on the lower right molars 5 minutes per day with a 0.3 g acceleration and peak strain of 30 με registered by accelerometer and strain gauge. The static load group received an equivalent magnitude of static force (30 με). The control group did not receive any treatment. Samples were collected at days 0, 28, and 56 for reverse transcriptase polymerase chain reaction analysis, microcomputed tomography, and histology and fluorescent microscopy analysis.
Our experiments showed that dynamic loading had a striking effect on condylar cartilage, increasing the proliferation and differentiation of mesenchymal cells into chondrocytes, and promoting chondrocyte maturation. This effect was accompanied by increased endochondral bone formation resulting in lengthening of the condylar process.
Low-magnitude, high-frequency dynamic loading can have a positive effect on condylar cartilage and endochondral bone formation in vivo. This effect has the potential to be used as a treatment for regenerating condylar cartilage and to enhance the effect of orthopedic appliances on mandibular growth."
A longitudinal study of arch size and form in untreated adults
"Adulthood—the lengthy phase following attainment of biologic maturity—often is perceived as a period of “no change” or one of slow deterioration. Recent skeletodental studies discount this stereotype. Changes in arch size and shape were studied here in a longitudinal series of 60 adults with intact dentitions. Full-mouth study models were taken at about 20 years of age and again at about 55 years. Some variables—particularly those between arches (incisor overbite and overjet, molar relationship) and mandibular intercanine width—remained age-invariant. In contrast, all other measures of arch width and length changed significantly (P<0.01): Arch widths increased over time, especially in the distal segments, whereas arch lengths decreased. These changes significantly altered arch shape toward shorter-broader arches. The data suggest that changes during adulthood occur most rapidly during the second and third decades of life, but do not stop thereafter. Possible mechanisms driving these changes in tooth position are discussed."
"Dental casts were taken on 60 older adults"
Figure 2 shows arch width and length.
Continuing bone growth throughout life: A general phenomenon
"Cross-sectional data on 2799 subjects from five different populations and longitudinal data on 113 older adults indicate continuing adult bone growth in the second metacarpal. Similar 6-decade increases in the size of the cranium confirm continuing bone growth as a general phenomenon not necesarily related to weightbearing or flexion stress and representing an increase of approximately 10% in skeletal volume concomitant with the major age-associated decrease in skeletal mass."
"there is a small but completely systematic three-decade gain in metacarpal width at mid-shaft in both sexes and all five populations sampled"
The scientists reported an increase in skull length.
"Modeling-based bone formation contributes to the periosteal expansion, just as remodeling-based resorption is responsible for the medullary expansion seen at the long bones with aging."<-Can we translate this into height?
"Odanacatib inhibits bone resorption by inhibiting cathepsin K activity, whereas modeling-based bone formation is stimulated at periosteal surfaces. Inhibition of sclerostin stimulates bone formation and histomorphometric analysis demonstrated that bone formation is predominantly modeling based."
"Strain alone can induce a significant increase in bone morphogenetic protein 2 (BMP2) mRNA levels in human BM-MSPCs without any addition of osteogenic supplements"
"Excessive strain causes regional microdamage, which leads to targeted remodeling removing the damaged bone and a larger volume of the surrounding undamaged bone, this temporary volume deficit increases the strain in neighboring bone and the potential establishment of a vicious cycle between damage and repair"
"Bone modeling has been demonstrated in aging humans. Modeling-based bone formation contributes to the periosteal expansion, just as remodeling-based resorption is responsible for the medullary expansion seen at long bones and ribs with aging"
"Osteocytes are terminally differentiated osteoblasts which become embedded in newly formed bone matrix and produce sclerostin. Sclerostin binds to lipoprotein-related peptide (LRP) 5/6 and thereby inhibits LRP5/6 from binding to the frizzled receptor and activating the Wnt pathway"
Extreme elongation of the transverse processes of the fifth lumbar vertebra: an unusual variant.
"The fifth lumbar vertebra has massive transverse processes that are continuous with the pedicle and encroach the body of the vertebra. These processes are mainly meant for the attachment of the iliolumbar ligament. With increasing age, the iliolumbar ligament can undergo secondary degenerative changes such as calcification, hyalinization, and myxoid degeneration. [We discovered an] extremely elongated transverse processes of the fifth lumbar vertebra in a 45-year-old woman who underwent surgery for an intervertebral disc herniation. This unusual variant may be caused by calcification of the iliolumbar ligament rather than a congenital anomaly."
Causing calcification of ligaments isn't really reproducible but it's still bone length increase in a 45 year old.
If you look figure 1A and 1B you can see that the increase in transverse process is insane with the elongated transverse process being about 3 times longer than the other bones.
"[There was] a calcified nodular lesion in the left pelvic cavity, suggesting the presence of a calcified uterine myoma[mesenchymal tumor]."
"the trabecular bone of the transverse processes have normal shape and length, and the compact bone is elongated."
"[There was] a large, extruded intervertebral disc on the right side, compressing the dural sac."
"the direction of elongation of the transverse process corresponded to the position of the iliolumbar ligament." Thus providing evidence that the iliolumbar ligament was calcified.
"The iliolumbar ligament is attached to the tip and the anteroinferior aspect of the transverse processes of the fifth lumbar vertebra"<-So the ligament may have been used as a scaffold to grow the bone longer. Maybe a ligament can be inserted into a long bone so you can grow taller forever.
Mechanical strain leads to condylar growth in adult rats.
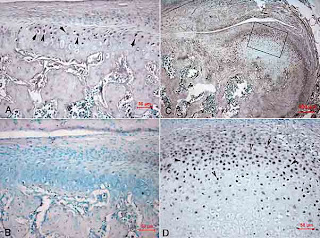
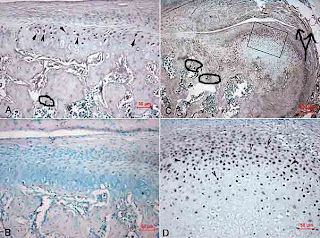
"Mechanical strain produced by forward mandibular positioning was found to enhance mandibular condylar growth in experimental animals and in patients. [We] identify the changes in number and rate of the proliferating mesenchymal cells in mandibular condyles of adult rats and to correlate these changes to the expression of SOX9 and type II collagen under mechanical strain. Seventy-eight 120-day-old female Sprague-Dawley rats{rats generally stop growing at six months} were randomly allotted to six groups, nine animals in each experimental group according to different time points. Cell kinetic studies for expression of PCNA were used to identify number and rate of proliferating mesenchymal cells. Immunostaining of SOX9 and in situ hybridization of Col2a1 gene were carried out. Results showed a significant increase in number of replicating mesenchymal cells and proliferation rate. The expression of SOX9 was enhanced and Col2a1 gene transcript was then activated. The proliferative layer became thicker on experimental day 21. The thickness of chondroblast layer and chondrocyte layer showed significant increase from experimental day 14 to day 30. Mechanical strain produced by mandibular advancement in adult rats promotes the proliferation of mesenchymal cells. Under control of transcription factor SOX9, these mesenchymal cells are then committed to enter the chondrogenic route leading to condylar growth."
Producing proliferating of MSCs which then differentiate into chondrocytes via SOX9 is exactly what we're trying to accomplish with LSJL.
"mandibular advancement reactivates endochondral ossification in the posterior condyle and ultimately results in new bone formation in the condyle"
"mandibular advancement reactivates endochondral ossification in the posterior condyle and ultimately results in new bone formation in the condyle"
"In the adult patients treated with Herbst appliance this would be the result of a reactivation of cells of prechondroblast zone, thus representing an area of active condylar growth"
"continuous bite jumping devices induce morphological adaptation in the mandible especially the length of condylar head in adult rats"
"During mandibular growth, the condyle undergoes endochondral ossification and the condylar cartilage acts as a template for bone growth. However, in the adults, the remnant condylar cartilage serves more 'articular' function than 'growth' function. From growing to adults, the thickness of cartilage becomes thinner. It has been reported that the adult rat's condyle is covered by a thin layer of cartilage, which is composed of 2-3 layers of chondrocytes and there is no obvious hypertrophic layer in the cartilage since a weak staining of Type X collagen, the marker of endochondral ossification, was obscured. This result implies that adult rat condyle stops growth or becomes inactive of endochondral ossification. Bone growth in the condyle is closely related to cartilage formation in the growing rats"
"The fibrous zone of the condylar cartilage of adult rats is composed of several layers of flattened cells . The cells in the proliferative layer, which was densely packed, located beneath the fibrous layer . Underneath the proliferative layer, the cells became chondrospecific and flattened gradually. The extracellular matrix was positively stained with type II collagen and thus this layer was termed as "type II collagen positive layer" in the present stud which may represent the level of expression of type II collagen. The current study showed that the thickness of cartilage in posterior condyle was apparently affected by the bite-jumping device. Analysis showed the thickness of each layer of cartilage in controls was unchanged during the observation period. In the experimental group, there were significant changes observed in all the layers. The thickness of fibrous layer showed significant increase from day 14 of mandibular advancement and was maintained from day 30 to day 60 Mandibular advancement resulted in an increase in the thickness of the proliferative layer on day 21 which was then followed by a decrease to the level found in the matched controls. The thickness of type II collagen positive layer showed a significant increase from experimental day 14. The highest level was presented on experimental day 21 followed by a lower level on day 30. The level of expression of type II collagen expressed on day 60 returned to the level expressed in the controls."
"The population [of MSCs] in that of mandibular advancement groups was significantly increased on day 21" No differences were observed in the control group.
"In the control groups, only a few SOX9 positive cells existed in the proliferative layer. On experimental day 3, SOX9 positive cells were remarkably increased in the proliferative layer of experimental animals. On experimental day 21, the SOX9 positive cells were increased in both proliferative layer and chondroblast layer but no positive staining can be detected in the hypertrophic chondrocyte"
"mandibular advancement in adult rats resulted in increase in condylar growth as measured by a significant increase in: the number and rate of replicating mesenchymal cells; the expression of transcription factor SOX9, the factor that regulates mesenchymal cell differentiation into chondroblasts; the thickness of cartilage layers and finally increase in the amount of osteocytes that led to increase in the production of new bone in the adult condyles "
a forward biting jump appliance is only similar to LSJL if the joint loading done by LSJL is similar to the pull by that of the lateral pterygoid muscle.
"[The] significant increase in SOX9 expression level coincided with the rate of proliferation of mesenchymal cells"
It should be noted that the population of MSCs began to decline after thirty days. That may be related to an adaptative response and indicates that there may need to be a deconditioning period with LSJL after 30 days.
" Each group consisted of nine rats with bite-jumping appliances and four untreated controls"
On this page is an example of a bite jumping appliance(It's the Herbst) mentioned earlier.
Here's the picture of experimental jaw versus control:
"Alcian blue-PAS staining showing the overview of rat's TMJ condyle at age of 141-day (experimental day 21). The thickness of cartilage in the posterior condyle is remarkably increased by mandibular advancement (B) than that of control (A). Two measurement frames are illustrated on (B), one for the measurement of thickness of layers (1104×811µm, black) and the other frame for the cell counting (547×402µm, red)."
Here's the ectopic chondrogenesis highlighted with GIMP(blue line):
Here's the Col2a1 expression areas:
"In situ hybridization showing the localization of type II collagen (Col2a1) mRNA (marked with arrow) in the condylar cartilage of control (A) and experimental animal (C.D) on experimental day 21. (D) is higher magnification of (C). In situ hybridization with sense probe shows no hybridization signal in the cartilage (B)." So there was no active COL2A1 mRNA production in B which is the control.
Arrows point to two possible areas where the bone ends both are distant from the Col2a1 staining indicating that the new growth plate formation is within the bone thus providing evidence for proof of concept for LSJL to form new growth plates within bone.Here's another paper with the same author:
" sagittal deviation using the postural hyperpropulsor on male rats from the age of 48 to 180 days, which resulted in greater length of mandible than that of control. Experiments of continuous bite-jumping in young rats resulted in enhanced mandibular growth and remodeling of the glenoid fossa"
"Fifty-two 120-day-old nongrowing female Sprague-Dawley rats were included in this study."
"mandibular advancement could also stimulate the adaptive growth of the condyle in adult rats. This finding does not support previous experimental results where it was reported that adult monkeys lost the ability for condylar remodeling. The possible reason may be that the stage of dentition could not reflect the exact chronological age of experimental monkeys."
"Because there was no increase in the length of the mandibular base, the remodeling of the condyle ultimately resulted in the increase in mandibular length "
Let's look at one of the studies that shows that monkeys lost the ability to grow in mandible length with age:
<-in this study the authors speculate it is perhaps a deficit in neuromuscular function that made the monkeys unable to move the jaw forward enough to stimulate growth and not due to capacity(I am not able to copy and paste the study).
The study won't let me copy and paste. When I get a chance, I might print the paper out and scan the images in. Click on the link and look at figure 2 for new cartilage growth. Note in figure 2a that the region of new cartilage formation pointed to by the arrow is disconnected from the rest the cartilage. Also note that there is red staining in scattered quantities throughout the entirety of the epiphysis with the exception of that attached to the bone attached to the new red zone.
Note that in figure 1 there is staining for Type II Collagen deep within the epiphysis in the control group.
In figure 3a there is staining for Type II collagen throughout the entire bone. If you look at figure five bone formed downward furthering the possibility that you can increase bone length via the articular cartilage.
If you look at figure 5 you can see the new bone formation.
If you look at figure 6, it took until about day 21 to start seeing results and results decreased at day 60 so there could be an adaptive mechanism.
It would be interesting to note if intermittent mandibular forward positioning could result in the same objective.
"Advancement of the calcification front in the cartilage, which is a measure of the growth of the cartilage, can be determined by the administration of two dose bone‐markers at specific intervals. It appears that growth still takes place in animals of 12–18 months. This growth is possible by the persistence of chondrogenic cells. The overall growth of the central part of the condyle amounts to about 2 mm over the period from 2 to 18 months.
Raising of the bite in the rat has an obvious influence on the temporomandibular joint, and on the condyle in particular. Within a few days an increase of growth‐rate of cartilage can be demonstrated. This extra growth is temporary, and the intensity and duration of the response is determined by the age of the animal. This adaptation is related to the presence of chondrogenic cells in the cartilaginous layer in the condyle."
"The aim of this investigation was to assess quantitatively the adaptive changes in the condyles of adult rats to forward mandibular positioning. The level of types II and X collagen expressed in the condyles of adult rats was compared with that formed in response to forward mandibular positioning and the levels of expression were correlated to the amount of bone formed in response to mandibular advancement. Seventy-eight 120-day-old female Sprague-Dawley rats were included in this study. The rats were randomly allocated to six groups. Each group consisted of nine rats with bite-jumping devices and four untreated controls. The animals in each group were sacrificed on days 3, 7, 14, 21, 30, and 60. Immunostaining was used for the detection of types II and X collagen, while Alcian blue-PAS was used to observe the extracellular matrix and new bone formation. New cartilage was formed in the posterior condyle. The highest level of expression of types II and X collagen were present on day 21, the amount of increase was 247.99 and 540.08 per cent, respectively. The highest level of new bone formation was measured at day 30 of advancement when the amount of increase in new bone formation was 318.91 per cent. Forward mandibular positioning causes changes in the biophysical environment of the temporomandibular joint (TMJ) of adult rats that leads to condylar adaptation."
The rats were advanced 4 mm in continuous advancement. I don't know exactly what this means.
The rats were advanced 4 mm in continuous advancement. I don't know exactly what this means.
Note that in figure 1 there is staining for Type II Collagen deep within the epiphysis in the control group.
In figure 3a there is staining for Type II collagen throughout the entire bone. If you look at figure five bone formed downward furthering the possibility that you can increase bone length via the articular cartilage.
If you look at figure 5 you can see the new bone formation.
If you look at figure 6, it took until about day 21 to start seeing results and results decreased at day 60 so there could be an adaptive mechanism.
It would be interesting to note if intermittent mandibular forward positioning could result in the same objective.
"case of altered condylar morphology in adult male with temporomandibular disorders was reported in 30-year-old male patient. Erosion and flattening of the left mandibular condyle were observed by panoramic x-ray. The patient was treated with splint therapy that determined mandibular advancement. Eight months after the therapy, reduction in joint pain and a greater opening of the mouth was observed, although crepitation sounds during mastication were still noticeable."
"The mandibular condyle is an ovoidal bony structure that articulates with the temporal bone by means of a biconcave disk."
"Both articular surfaces are covered by a connective fibrous tissue (condylar cartilage). On the articular surface of the condyle, the collagen fibres are parallel to the condylar surface, and are in continuity with the fibrous layer of the periosteum.
The condylar cartilage covers very dense undifferentiated mesenchyme, within which are multipotential cells, forming either cartilage or bone, depending upon the environmental circumstances"<-the presence of this mesenchyme may not be present in other regions.
"Mandibular condylar cartilage is characterised histologically as fibrocartilage containing a layer of pre-chondroblastic mesenchymal stem cells which can undergo rapid differentiation into chondrocytes.
Other forms of mature articular cartilage do not have such progenitor cells and only poorly responsive chondrocytes "<-this is a problem. Though I do not think this is entirely true.
"subcondylar trabecular bone formation is apparently not affected by age"<-The study mentioned is
Induced growth of the mandibular condyle in the rat"Advancement of the calcification front in the cartilage, which is a measure of the growth of the cartilage, can be determined by the administration of two dose bone‐markers at specific intervals. It appears that growth still takes place in animals of 12–18 months. This growth is possible by the persistence of chondrogenic cells. The overall growth of the central part of the condyle amounts to about 2 mm over the period from 2 to 18 months.
Raising of the bite in the rat has an obvious influence on the temporomandibular joint, and on the condyle in particular. Within a few days an increase of growth‐rate of cartilage can be demonstrated. This extra growth is temporary, and the intensity and duration of the response is determined by the age of the animal. This adaptation is related to the presence of chondrogenic cells in the cartilaginous layer in the condyle."
"From the results it can be seen that an increase of the vertical dimension leads to a
temporary period of extra growth of the condyle. Not only is the chondrogenic zone
activated but the cartilaginous zone also reacts with heightening of its layer by production of cartilaginous substance
Cell and matrix response of temporomandibular cartilage to mechanical loading.
"The generation of transgenic mice expressing green fluorescent proteins (GFPs) has greatly aided our understanding of the development of connective tissues such as bone and cartilage. Perturbation of a biological system such as the temporomandibular joint (TMJ) within its adaptive remodeling capacity is particularly useful in analyzing cellular lineage progression. The objectives of this study were to determine: (i) if GFP reporters expressed in the TMJ indicate the different stages of cell maturation in fibrocartilage and (ii) how mechanical loading affects cellular response in different regions of the cartilage.
Four-week-old transgenic mice harboring combinations of fluorescent reporters (Dkk3-eGFP, Col1a1(3.6 kb)-GFPcyan, Col1a1(3.6 kb)-GFPtpz, Col2a1-GFPcyan, and Col10a1-RFPcherry) were used to analyze the expression pattern of transgenes in the mandibular condylar cartilage (MCC). To study the effect of TMJ loading, animals were subjected to forced mouth opening with custom springs exerting 50 g force for 1 h/day for 5 days. Dynamic mineralization and cellular proliferation (EdU-labeling) were assessed in loaded vs control mice.
Dkk3 expression was seen in the superficial zone of the MCC, followed by Col1 in the cartilage zone, Col2 in the prehypertrophic zone, and Col10 in the hypertrophic zone at and below the tidemark. TMJ loading increased expression of the GFP reporters and EdU-labeling of cells in the cartilage, resulting in a thickness increase of all layers of the cartilage. In addition, mineral apposition increased resulting in Col10 expression by unmineralized cells above the tidemark.
The TMJ responded to static loading by forming thicker cartilage through adaptive remodeling."
"new mineralized cartilage apposition within the 24-hour period"
Biomechanical behavior of the temporomandibular joint disc.
Here's a study on how progenitor cells in the cartilage may play a role in this process:
Progenitor Cells of the Mandibular Condylar Cartilage.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4613756/
"Articular cartilage has little regenerative capacity. Recently, genetic lineage tracing experiments have revealed chondrocyte progenitors at the articular surface. We further characterized these progenitors by using in vivo genetic approaches. Histone H2B–green fluorescent protein retention revealed that superficial cells divide more slowly than underlying articular chondrocytes. Clonal genetic tracing combined with immunohistochemistry revealed that superficial cells renew their number by symmetric division, express mesenchymal stem cell markers, and generate chondrocytes via both asymmetric and symmetric differentiation. Quantitative analysis of cellular kinetics, in combination with phosphotungstic acid–enhanced micro–computed tomography, showed that superficial cells generate chondrocytes and contribute to the growth and reshaping of articular cartilage. Furthermore, we found that cartilage renewal occurs as the progeny of superficial cells fully replace fetal chondrocytes during early postnatal life. Thus, superficial cells are self‐renewing progenitors that are capable of maintaining their own population and fulfilling criteria of unipotent adult stem cells. Furthermore, the progeny of these cells reconstitute adult articular cartilage de novo , entirely substituting fetal chondrocytes."
Regional shape change in adult facial bone curvature with age.
"Three-dimensional semilandmarks representing the curvature of the orbits, zygomatic arches, nasal aperture, and maxillary alveolar process were collected from a cross-sectional cranial sample of mixed sex and ancestry (male and female; African- and European-American), partitioned into three age groups (young adult = 18-39; middle-aged = 40-59 years; and elderly = 60+ years). Each facial region's semilandmarks were aligned into a common coordinate system via generalized Procrustes superimposition. Regional variation in shape was then explored via a battery of multivariate statistical techniques. Age-related shape differences were detected in the orbits, zygomatic arches, and maxillary alveolar process."
"adult craniofacial curvature shape is not static throughout human life. Instead, age-related spatial modifications occur in various regions of the craniofacial skeleton."
"Increases in craniofacial dimensions such as facial height, mandibular length, bizygomatic and bigonial breadth, and head circumference, length, and breadth have been detected with advancing age"
Natural craniofacial changes in the third decade of life: a longitudinal study.
"Natural head position lateral cephalometric films and dental casts of 30 people (14 women and 16 men) were evaluated. The mean age at the beginning of the observation period was 22.35 years for the women and 22.19 years for the men, and the observation period was approximately 10 years. Cephalometric films were superimposed by the structural method, and the measurements of the dental casts were made with a digital caliper. All tracings were digitized, and changes in the 65 cephalometric and 10 dental cast measurements were evaluated statistically. In this early adult period, small changes were found in the craniofacial and craniocervical parameters; the changes were more significant in the women. The most significant changes were found in the vertical dimension. The total anterior face height increased in both genders, while the lower anterior face height increased significantly in the female group. Soft tissue measurements reflected the vertical skeletal changes. The retrusion of the upper lip was significant in the women, and the upper lip thickness decreased in both genders. In the dentoalveolar region, the main movement was eruption of the teeth. The overbite amount increased significantly only in the female group. All dental arch measurements decreased in both sexes. The decrease in the mandibular arch length discrepancy was significant in the men."
Adult Growth, Aging, and the Single-Tooth Implant.
Effects of mechanical loads on surface morphology of the condylar cartilage of the mandible in rats., "Hard-diet condyles had a rougher, more porous articular surface while soft/hard-diet condyles were intermediate between nonporous and slightly roughened condyles. None of the condyles showed ridges or elevations on the articular surface. Sex, age and time of the diets did not significantly affect these results."
Cell and matrix response of temporomandibular cartilage to mechanical loading.
Four-week-old transgenic mice harboring combinations of fluorescent reporters (Dkk3-eGFP, Col1a1(3.6 kb)-GFPcyan, Col1a1(3.6 kb)-GFPtpz, Col2a1-GFPcyan, and Col10a1-RFPcherry) were used to analyze the expression pattern of transgenes in the mandibular condylar cartilage (MCC). To study the effect of TMJ loading, animals were subjected to forced mouth opening with custom springs exerting 50 g force for 1 h/day for 5 days. Dynamic mineralization and cellular proliferation (EdU-labeling) were assessed in loaded vs control mice.
Dkk3 expression was seen in the superficial zone of the MCC, followed by Col1 in the cartilage zone, Col2 in the prehypertrophic zone, and Col10 in the hypertrophic zone at and below the tidemark. TMJ loading increased expression of the GFP reporters and EdU-labeling of cells in the cartilage, resulting in a thickness increase of all layers of the cartilage. In addition, mineral apposition increased resulting in Col10 expression by unmineralized cells above the tidemark.
The TMJ responded to static loading by forming thicker cartilage through adaptive remodeling."
"Unlike most hyaline articular cartilages in the appendicular joints, the MCC is classified as fibrocartilage "
"new mineralized cartilage apposition within the 24-hour period"
If you look at figure 3 you can see signs of increased endochondral ossification.
"The TB signal extended into in the mineralized cartilage zone and protruded further into the subchondral bone in the loaded group."
"loading enhances the accumulation of mineralized cartilage resulting in a greater separation of the unmineralized cartilage from the subchondral bone."<-this seems to indicate that maybe endochondral ossification did not occur. And only cartilage mineralization.
Biomechanical behavior of the temporomandibular joint disc.
"The temporomandibular joint (TMJ) disc consists mainly of collagen fibers and proteoglycans constrained in the interstices of the collagen fiber mesh. This construction results in a viscoelastic response of the disc to loading and enables the disc to play an important role as a stress absorber during function. The viscoelastic properties depend on the direction (tension, compression, and shear) and the type of the applied loading (static and dynamic). The compressive elastic modulus of the disc is smaller than its tensile one because the elasticity of the disc is more dependent on the collagen fibers than on the proteoglycans. When dynamic loading occurs, the disc is likely to behave less stiffly than under static loading because of the difference of fluid flow through and out of the disc during loading. In addition, the mechanical properties change as a result of various intrinsic and extrinsic factors in life such as aging, trauma, and pathology. Information about the viscoelastic behavior of the disc is required for its function to be understood and, for instance, for a suitable TMJ replacement device to be constructed. In this review, the biomechanical behavior of the disc in response to different loading conditions is discussed"
"The articular surfaces of the TMJ are highly incongruent. Due to this incongruence, the contact areas of the opposing articular surfaces are very small. When joint loading occurs, this may lead to large peak loads, which may cause damage to the cartilage layers on the articular surfaces. The presence of a fibro-cartilaginous disc in the joint is believed to prevent these peak loads since it is capable of deforming and adapting its shape to that of the articular surfaces. These deformations ensure that loads are absorbed and spread over larger contact areas. In addition, the shape of the disc and the area and location of its contact areas with the articular surfaces change continuously during jaw movement to adapt to the changing geometry of the articular surfaces of the mandible and temporal bone."
" while translation of the condyle in the forward direction to obtain a protrusive or open jaw position leads to a concentration of the deformation in the lateral part of the disc."
"When the disc is compressed or stretched in one direction, not only will it deform in that direction (primary strain), but it will also become thicker or thinner, respectively, in a direction perpendicular to it (secondary strain). "
"the small permeability of the collagen network impedes interstitial fluid flow through this network. Therefore, the loads acting on a cartilaginous structure as the disc are initially transmitted by a pressurization of the incompressible fluid without much deformation of the collagen network. Nonetheless, fluid flow through the collagen network leads to a gradual transfer of the load from the fluid to the collagen fibers. When further loaded, the collagen network deforms, and water is squeezed out of the disc while the orientation of the collagen fibers is re-arranged "
"The movement of fluid out of the disc and the re-arrangement of the collagen fibers are reversible when the disc is not deformed beyond the physiologic strain range. Even application of significant long-term stresses beyond the physiologic strain range introduces but minor changes in fiber waviness and alignment within the disc. This enables the disc to adapt its shape continuously to fit in the space between the opposing articular surfaces and to distribute loads suitably in the TMJ. Collagen gives the disc much of its tensile stiffness and strength. "
"mechanical stress affects the GAG synthesis in the disc, especially that of chondroitin sulfate, dermatan sulfate, and hyaluronic acid. Static loading decreases the proteoglycan synthesis in cartilaginous structures, whereas dynamic loading is positively related to this synthesis and is considered as an important factor for maintenance of the homeostasis of the joint cartilage "<-maybe because dynamic loading drives fluid flow and allows more nutrients to get in?
Here's a study on how progenitor cells in the cartilage may play a role in this process:
Progenitor Cells of the Mandibular Condylar Cartilage.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4613756/
"The secondary cartilage of the mandibular condyle is unique as it undergoes endochondral ossification during growth and robustly remodels in response to changes in its mechanical loading environment. This cartilage is derived from mesenchymal progenitor cells that express markers of early osteoblast differentiation, namely alkaline phosphatase (ALP) and runt-related transcription factor 2 (Runx2). Interestingly, these progenitor cells then differentiate into cartilage with appropriate mechanical loading. these cells can be labeled by osteoblast progenitor cell markers, including the 3.6 fragment of the rat collagen type 1. However, the role these mesenchymal progenitor cells play in adult mandibular condylar cartilage maintenance and adaptation, as well as the existence of a more potent progenitor cell population within the mandibular condylar cartilage, remain in question. Further characterization of these cells is necessary to determine their potency and regenerative capacity to elucidate their potential for regenerative therapy."
"After the cessation of growth, the mandibular condylar cartilage becomes phenotypically similar to other articular cartilages by entering into a post-mitotic state"
"there still appears to be a progenitor cell population capable of reactivating in response to changes in mechanical loading"<-where these progintor cells are present in other articular cartilage is the question.
Progenitor cells in other articular cartilage types:
Origin and function of cartilage stem/progenitor cells in osteoarthritis.
Progenitor cells in other articular cartilage types:
Origin and function of cartilage stem/progenitor cells in osteoarthritis.
"Articular cartilage is a physiologically non-self-renewing avascular tissue with a singular cell type, the chondrocyte, which functions as the load-bearing surface of the arthrodial joint. Injury to cartilage often progresses spatiotemporally from the articular surface to the subchondral bone, leading to development of degenerative joint diseases such as osteoarthritis (OA). Although lacking intrinsic reparative ability, articular cartilage has been shown to contain a population of stem cells or progenitor cells, similar to those found in many other adult tissues, that are thought to be involved in the maintenance of tissue homeostasis. These so-called cartilage-derived stem/progenitor cells (CSPCs) have been observed in human, equine and bovine articular cartilage, and have been identified, isolated and characterized on the basis of expression of stem-cell-related surface markers, clonogenicity and multilineage differentiation ability. However, the origin and functions of CSPCs are incompletely understood. We review here the current status of CSPC research and discuss the possible origin of these cells, what role they might have in cartilage repair, and their therapeutic potential in OA."
"mild enzymatic insult to the cartilage ECM promoted CPCs migration in cultured articular cartilage explants."
Superficial cells are self‐renewing chondrocyte progenitors, which form the articular cartilage in juvenile mice
Superficial cells are self‐renewing chondrocyte progenitors, which form the articular cartilage in juvenile mice
<-We need to know how effective these stem cells are at self renewing as adults for adult height increase via articular cartilage.
"whereas deep articular chondrocytes in adult mice are derived from cells that were initially at the cartilage surface in newborn mice, which is consistent with appositional growth, beneath the surface cartilage, growth is also interstitial"
"superficial cells are slow-dividing progenitors of middle and deep zone chondrocytes"
"whereas deep articular chondrocytes in adult mice are derived from cells that were initially at the cartilage surface in newborn mice, which is consistent with appositional growth, beneath the surface cartilage, growth is also interstitial"
"superficial cells are slow-dividing progenitors of middle and deep zone chondrocytes"
Regional shape change in adult facial bone curvature with age.
"Three-dimensional semilandmarks representing the curvature of the orbits, zygomatic arches, nasal aperture, and maxillary alveolar process were collected from a cross-sectional cranial sample of mixed sex and ancestry (male and female; African- and European-American), partitioned into three age groups (young adult = 18-39; middle-aged = 40-59 years; and elderly = 60+ years). Each facial region's semilandmarks were aligned into a common coordinate system via generalized Procrustes superimposition. Regional variation in shape was then explored via a battery of multivariate statistical techniques. Age-related shape differences were detected in the orbits, zygomatic arches, and maxillary alveolar process."
"adult craniofacial curvature shape is not static throughout human life. Instead, age-related spatial modifications occur in various regions of the craniofacial skeleton."
"Increases in craniofacial dimensions such as facial height, mandibular length, bizygomatic and bigonial breadth, and head circumference, length, and breadth have been detected with advancing age"
Natural craniofacial changes in the third decade of life: a longitudinal study.
"Natural head position lateral cephalometric films and dental casts of 30 people (14 women and 16 men) were evaluated. The mean age at the beginning of the observation period was 22.35 years for the women and 22.19 years for the men, and the observation period was approximately 10 years. Cephalometric films were superimposed by the structural method, and the measurements of the dental casts were made with a digital caliper. All tracings were digitized, and changes in the 65 cephalometric and 10 dental cast measurements were evaluated statistically. In this early adult period, small changes were found in the craniofacial and craniocervical parameters; the changes were more significant in the women. The most significant changes were found in the vertical dimension. The total anterior face height increased in both genders, while the lower anterior face height increased significantly in the female group. Soft tissue measurements reflected the vertical skeletal changes. The retrusion of the upper lip was significant in the women, and the upper lip thickness decreased in both genders. In the dentoalveolar region, the main movement was eruption of the teeth. The overbite amount increased significantly only in the female group. All dental arch measurements decreased in both sexes. The decrease in the mandibular arch length discrepancy was significant in the men."
"Single-tooth implants are an increasingly popular method for replacing single teeth. While the effects of growth on implants in children have been well documented, the changes that occur in adults have not been studied with respect to single-tooth implants. It has been assumed that adults are stable and do not change; however, research in the last few years has indicated that adults do change with aging, and adult growth does occur. The changes in adults occur over decades rather than rapidly, as seen in children. Aging changes are readily apparent in the soft tissues of the face and create dramatic changes. Changes in the jaws and teeth occur as a result of continued, slow growth, in contrast to the aging effects seen in soft tissues. Growth changes occur in the arches and result in adaptive changes in the teeth over time, both vertically and horizontally, and in alignment. These dental changes may result in a lack of occlusion vertically or malposition of adjacent natural teeth relative to the implant crown. Clinicians may be well advised to observe and report these changes and warn patients that changes can occur over the service life of the implant-supported crown. These changes may require maintenance adjustments or possible remaking of the implant crown as a result of adult growth, wear, or the esthetic changes of aging."
"the myth
of “adults don’t grow” was put to rest. Although the
effects of adult growth are very slow and measured
in terms of decades, changes do occur"
"Between 15 and 25 years, males increase their
standing height by 15%, their maxillary depth by
20%, and their mandibular depth by 26%, while
positioning their mandible forward by 30% and
changing their maxillomandibular relationship by
33%"
"Underlying the soft tissue changes, skeletal changes
also occur in adults. The skeletal changes
appear more like the growth seen during adolescence"
"Since nearly all of the facial sutures
close in early adulthood, the skeletal growth during
adulthood must take place as a result of remodeling. Facial height increases both anteriorly and
posteriorly, with a greater increase in the lower than
in the upper face, resulting in a significant change in
the area of the dentition. This increase in
facial height totals nearly 3 mm between 17 and 80
years, with the increase continuing into the
eighties"
"While the average maxillary change is
small (1 mm) over a 60-year period, some individuals demonstrate as much as a 5-mm change.
Changes in mandibular position and length also
occur with increasing age. The symphysis[a fibrocartilagenous fusion between two bones] moves downward and forward throughout all age
spans, with males growing more than females."
The mandibular ramus continues to grow.




 From
From 
